Recommended Products
Hycosan Blue
Recommended artificial tears
Heat mask
Helps unblock glands
Lid wipes
Cleans lid crusting
Blepharitis
Blepharitis: What is blepharitis?
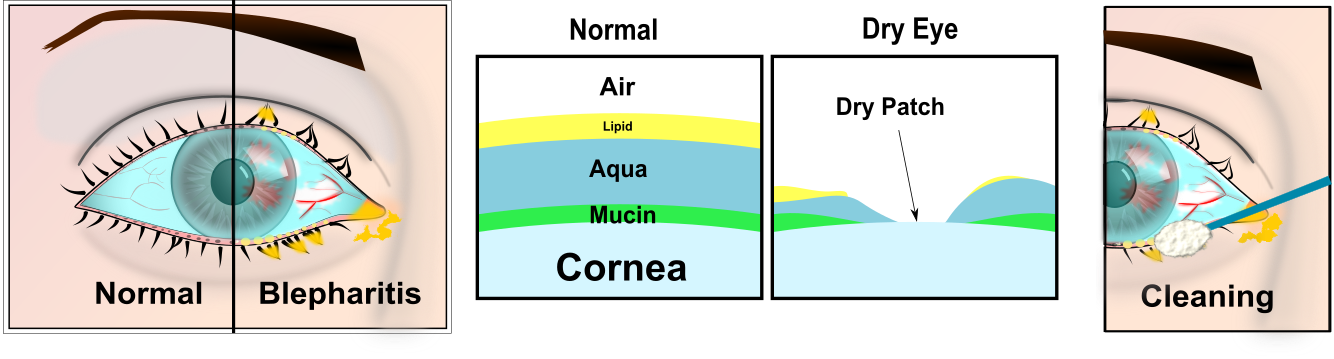
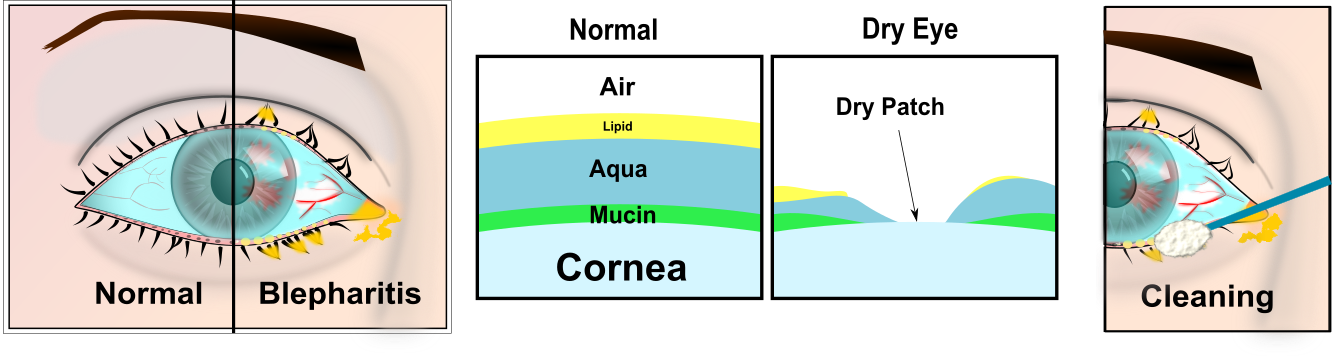
Blepharitis is the medical term for inflamed eyelids.
You may notice tired, or gritty eyes, which may be uncomfortable in sunlight or a smoky atmosphere. They may be slightly red, and feel as though there is something in them.
What is the cause of blepharitis?
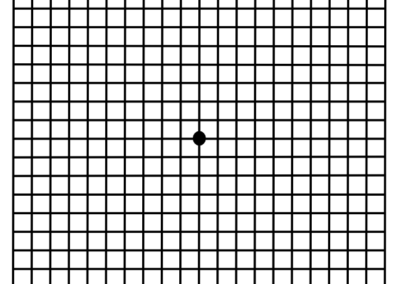
The eyelids have tiny glands in them, especially the lower lids. These glands make lipids that provide a protective oil coating over the tear film and helps stop the tears from breaking up.
As you get older, and particularly if you have dry skin, these glands can block. Without the substance that makes the tears spread, the tears break up, and dry patches develop. These patches make the eyes feel sore or gritty.
Aims of blepharitis treatment:
- to unblock the glands in the eyelid, which may be infected and inflamed, like acne on the face or a tiny boil.
- to replace tears if the eyes are dry.
The treatment will your eyes more comfortable, but there is no magic cure and it may return once treatment is ceased. Even with treatment your eyes may remain a little sore, but no harm will come to them and there is nothing to worry about. It’s not a serious condition, and there is rarely any damage to your eyes.
1 Lid Cleaning
Soak some cotton wool in warm water. Rub the cotton wool over the closed eyelids for 2-3 minutes, and repeat. Then clean the edge of the lower eyelid with a cotton bud to remove scales and debris on the edge of the eyelid. Move the cotton bud along the eyelid, using a mirror, and pulling the lid away from the eyeball with the fingers of the other hand. Rub the edge of the lid gently. The warm bathing helps to soften up the scales first. It is preferable to boil the water first to sterilise it, and allow it to cool. It may be two weeks for any improvement. Bathe 2-3 times a day, gradually reducing the frequency of bathing as the eyes become more comfortable (although bathing does not help everyone). It is safe to stop cleaning, but you may need to start again if the condition returns. There is a number of dedicated lid hygiene wipes and cleaners such as “Supranettes”, “Lidcare” and “Ocusoft Lid Cleaning Foam.” These are embedded with special cleaning agents which specifically target the secretions produced by blepharitis. Ask at the reception desk for details.
2 Lubricants
Lubricants can helpful to both assist the spread of your own tears and lubricate the eye, and replace tears if you have ‘dry eyes’. gels such as ‘Celluvisc’ or ‘Viscotears’ are usually helpful. drops such as ‘Systane’ or ‘Blink Intensive Eye Drops’ may help. Lipid replacement sprays, such as actimist, in some cases can help.
3 Warm Compresses
The lipids produced by the glands in the lids tend to be liquid at body temperature (36 degrees C). As the lids are exposed they tend to be a bit cooler and the lipids solidify. This leads to the lipids not spreading so well blocking the glands and allowing bacteria to inhabit the lash margins and glands. The bacteria can then release endotoxins into the the tears which can make the eyes feel uncomfortable, itchy and burning. Warm compresses will increase the temperature of the lipids to flow more like a liquid which will help unblock the glands.
4 Antibiotic ointment/Antibiotic tablets
If the cleaning is not helpful, an antibiotic ointment may be required from your GP. Try it for 3 months (chloramphenicol or fucithalmic). As the condition can return once treatments are stopped, you may need a repeat prescription from your GP. In severe blepharitis, antibiotic tablets may be an option, especially if associated with skin condition, such as acne rosacea, or very dry skin, or if the edge of your eyelid stays red with many scales. Antibiotic tablets are NOT suitable for everyone, particularly if you use several other tablets or have stomach problems. You will need to discuss this treatment with your GP first. Oxytetracycline 250mg twice daily (or doxcycline 50mg once daily [or erythromycin]) is usually used for 3 months. The benefit lasts several months after this treatment, but you may need to use further lid hygiene to stop recurrence.
Other causes of sore eyes
If you continue to have symptoms we recommend that you have your eyes assessed. You may have dry eyes (or at least poorly spreading tears) and replacement tears may help, as described. You may have an allergy, particularly if the eyes are itchy: Optichrom or another anti-allergy drop could help with these symptoms. You can see your GP on the NHS or alternatively, you can book in for a private Dry Eye Assessment with your Optometrist. Your eyes should be checked routinely by an optometrist for other conditions such as glaucoma; occasionally new spectacles may make the eyes more comfortable. If your eyes remain red and very irritable we can now offer DRY EYE ASSESSMENTS for £35.00 which can investigate the causes. Alternatively you can see your GP for NHS treatment.
BlephEx

BlephEx Treatment £40.00
Until recently Blepharitis was very hard to manage. Now there is the BlephEx. The First and Only Clinician Treatment for Blepharitis, is now available at Mellis Eyecare. BlephEx™ is a revolutionary new patented hand piece, used to very precisely and carefully, spin a medical grade micro-sponge along the edge of your eyelids and lashes, removing scurf and debris and exfoliating your eyelids.
BlephEx
Cleans the lids
BlephEx
Helps unblock glands
Dry Eye
Dry Eyes
Do you have ‘dry eyes’?
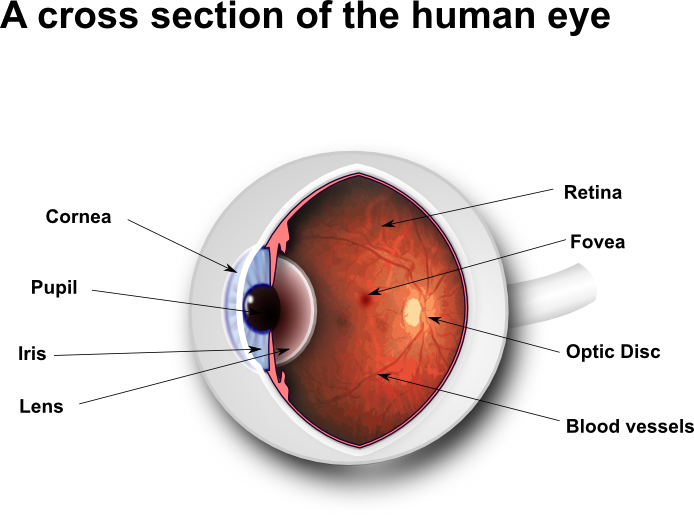
If your eyes feel tired, sore or gritty, you may have ‘dry eyes’. ‘Dry eyes’ occur when there are not enough tears to keep your eyes lubricated. Normally eyes are covered with a thin invisible film of tears. Tears are the lubricating ‘oil’ of the eye surface. If there are not enough tears, or if the tears do not spread properly across the eyes, the eyes become dry and sore.
They may feel ‘scratchy’ or gritty’, as though there is something in them. They may also be a little itchy, and they may be red. Poorly spreading tears may also be caused by ‘blepharitis’ (inflammation of the eyelids): see our leaflet on Blepharitis.
Sometimes your eyes may ‘water’; there may be enough tears, but the tears do not spread properly. The poor spreading makes the eyes sore, and this makes them water.
Having a dry eye does not damage your eye (unless the eye is extremely dry: see overleaf). Your sight may be slightly blurred, but will not be permanently affected.
Where are tears made normally?
Tears are made in a gland near the eyeball, and spread over the front of the eyeball, into tear ducts, and then into the nose.
The main cause of dry eyes is the drying up of the lacrimal gland. Anyone can develop dry eye, but it is more common in women, diabetes, and the over-45s. Usually the gland still produces tears, but not quite enough. Once damaged, the gland does not generally recover, but tear production can vary.
The gland may also be damaged by the body’s immune system. The immune system is meant to fight infections (‘germs’), but sometimes it becomes over-active. Whilst the immune system may damage the lacrimal gland, it does not damage the eye itself ‘Very dry eyes’.
What makes your dry eyes more Uncomfortable?
Your eyes may feel more sore in the wind, or any dry hot atmosphere. Contact lenses, or any thing that reduces blinking may make ‘dry eyes’ more uncomfortable, such as watching TV or a computer screen, or sewing.
There are fewer tears at night, so the eye may be sore and a little sticky in the morning. Disease of the eyelids stops the tears spreading properly, and makes the eyes sore. This is ‘blepharitis’: see the Blepharitis leaflet in this series. Some medicines reduce the amount of tears, such as tablets for depression and high blood pressure (eg water tablets).
Very dry eyes
This is a more serious condition, and a specialist should give you specific advice. The eye is prone to develop ulcers and infections. In addition to the treatment above (including frequent preservative-free drops and gel tears), the tear drainage ducts can be blocked with plugs (temporary) or cauterised to seal them (permanent). This saves the tears draining away, and makes the eyes a little more comfortable. Very dry eyes, especially if the mouth is dry as well, may be part of ‘Sjogrens’ sydrome: a dry mouth can lead to tooth decay. Sjogrens patients may also have joint problems.
What is the treatment of dry eyes?
To make your eyes comfortable you need to replenish the natural tear film that protects the surface of your eyes. There is no magic ‘cure’. Four types of products are available, and all are harmless: they do not contain any drugs, merely ‘oiling’ the surface of the eye.
Try the different products out. Your doctor can prescribe the products, and they can also be bought at pharmacies without a prescription. Some examples are listed next:
1 Tear drop preparations—in bottles
These are simple salt solutions with added ingredients that help them spread across the eye. They make the eye more comfortable by lubricating the surface, but the effect does not last all that long.
There are many types: different drops may suit different eyes,
so try different types. They are not very effective over night, and the eyes may be uncomfortable when you wake up. They also contain preservatives: this is only a problem if you have very dry eyes when the drops would need to be used quite frequently, and the dose of preservatives increases. Examples include ‘Liquifilm’, ‘Tears naturale’ and ‘Hypromellose’.
2 Eye gel preparations
These are relatively new products, and are the most useful. They last longer than drops, do not cause as much misty vision as ointments, and can be used at bedtime as they last partly through the night. There are two types: ‘Gel tears’ and ‘Viscotears’.
3 Eye ointments
These products are much thicker and greasier than eye drops. They stay in the eye much longer; try using them last thing at night. During the day they may cause misty vision. An example is ‘Simple’ eye ointment.
4 Tear drop preparations—without preservatives
These are particularly useful for people with very dry eyes. Because they have no preservative they can be used more often, upto every half an hour, without damaging your eyes. One example is ‘Minims’ tears: the ampoules (mini-bottles) contain about 14 drops, and may last a day with practice. They are moderately expensive.
We recommend Blink Intensive Eye Drops.
5 Eye drops which act like a gel
SYSTANE Lubricant Eye Drops contain a unique gelling and lubricating polymer system formulated to adjust to each patient’s individual tear film pH. This ensures optimum properties for each user and provides enhanced relief on a patient-to-patient basis.
It is like eyedrops but once on the eye SYSTANE behaves more like a gel mimicking the tear film more closely.
Summary of dry eye treatment
slightly dry eyes: drops in bottles or gels
moderately dry:gels (gel tears or viscotears)
severely dry: gels, ointments, occlude tear ducts (minor surgery),‘Minims’ artificial tears
Recommended Products
Blink Intensive
Recommended artificial tears
Heat mask
Helps unblock glands
Lid wipes
Cleans lid crusting
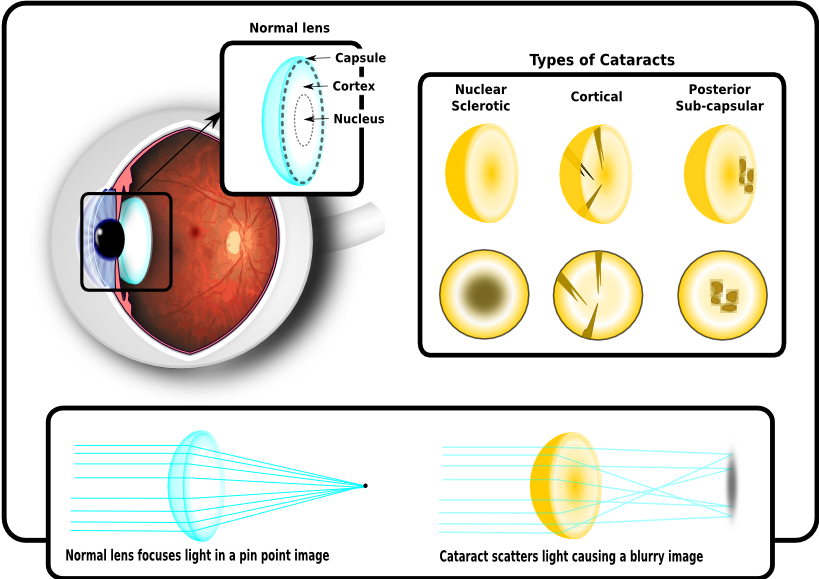
Cataracts: Cloudy lens
When you are young the lens has a lot of focusing power but as we age the lens continues to grow, hardens and gets less flexible and this normally leads to the need for reading glasses to assist our focusing at near. This continues through out our life and means the older we get the denser the lens gets. This makes it harder for light to travel through and more light is scattered, degrading the final image which lands on the retina.
The sort of problems that can occur are:
Problems with glare, i.e. bright sunlight or car headlights at night.
Blurred vision
Colours may be dull or washed out.
Problems detecting stairs or curbs
Once a cataract develops it rarely causes any permanent damage and if it starts to cause you problems there is a straight forward operation to restore normal vision. The lens is made up of several layers and it is the denser inner layers that normally cause a problem. An incision is made into the cornea and a hole is cut in the capsule, the outer layer of the lens. The middle part of the lens is liquefied using high frequency ultrasound and sucked out using a vacuum. Then an artificial lens is inserted into the eye, which rests within the capsule and restores normal vision. Spectacles may be required for clear distance and near vision.
Macula Degeneration
Dry & Wet Age Related Macular Degeneration
WEAR & TEAR (Age related changes)
The Macula is the area of the retina responsible for your most detailed vision. It is very energy intensive and with age this can cause a build up of waste material. This normally presents itself as yellow deposits within the retina called “drusen”.
Over many years these drusen can accumulate at the macula and cause a drop in your vision and this is termed Dry Age Related Macula Degeneration (Dry AMD). There is currently no treatment for this. The accumulation of waste materials is often accompanied by new vessels growing below the retina. These new vessels are the body’s way of helping the macula with its oxygen supply but unfortunately these vessels are fragile. This means that they can sometimes burst and spread in-between the retinal layers leading to distortion or a sudden vision loss which is termed Wet Age Related Macula Degeneration (Wet AMD).
When this happens it needs to be assessed as soon as possible as it may benefit from treatment using a cold laser (photocoagulation) or special eye injections.
What causes AMD?
The exact causes of AMD are still unknown but the following may have an influence:
- family links (possibly genetic or lifestyle)
- smoking & drinking.
- high blood pressure
- poor diet
- UV exposure
Regime for people at risk of AMD
- Alter diet to include more dark, green leafy vegetables, carrots and corn.
- Take over-the-counter slow release vitamin/mineral supplements with a meal.
- Wear blue light protective lenses and a cap or hat when outdoors.
- Consult GP for a comprehensive medical and treatment of any hypertension, hypercholesterolaemia or any other potentially compromising vascular disease.
- Seek professional help to achieve smoking cessation.
- Stop alcohol consumption.
- Check your vision regularly for distortion or central vision loss
- Nutrition and the eye: Age-related macular degeneration, Frank Eperjesi 2004
Some nutritional supplements are available that are designed to combat AMD. It is important to note that these nutrients are not a cure for AMD, nor will they restore vision already lost from the disease. However, they may play a role in helping certain people at high risk from developing advanced AMD. Ask your optician for more details.
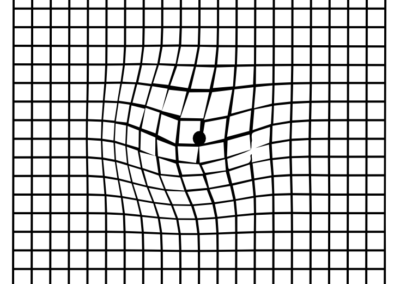
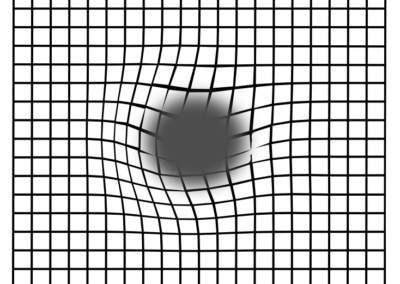
The Amsler Grid
The grid below is a quick and simple test, known as The Amsler Grid. It can help to determine whether you are experiencing the early symptoms of AMD, but remember it is not a substitute for an eye test.
Please follow these simple instructions now:
- Hold the grid around 12 inches (30cm) in front of your eyes.
- If you wear reading glasses leave them on but do not wear varifocals or distance glasses.
- Cover one eye with your hand and focus with your other eye on the centre dot.
- Check that you can see all four corners of the grid.
Example of Amsler Scotoma
If areas of the grid appear blurred, distorted, or in any way abnormal then you could be displaying the early signs of AMD. See your optician immediately.

What are floaters?
Flashing lights and Floaters
Often, people who have healthy eyes see floaters. They appear as spots, lines or cobweb effects, usually when you look at a plain surface such as a white wall or a clear blue sky. They often appear when the clear jelly in the main part of your eye gets older.
What are flashes?
Sometimes the jelly in the main part of your eye shrinks a little and tugs on the retina (the light-sensitive layer) at the back of your eye. This can cause flashes of light at the edge of your vision. These differ from the disturbance of vision that can occur with migraine.
When should I be concerned?
If you suddenly notice a shower of new floaters, or floaters along with flashes or a dark shadow or “curtain” in your vision, then you should seek advice urgently. These symptoms can mean that the retina is tearing. Go to an Accident and Emergency Department if necessary.
What will happen if the retina tears?
The retina is at the back of your eye. It receives the images and sends them to the brain. This is one of the things that enable you to see. If the retina tears, it may come away from the back wall of the eye. This is called retinal detachment. It can result in partial or complete loss of vision.
How is retinal detachment treated?
A tear may be treated by using a laser. If treated quickly, you may have a better chance of full recovery. However, if your retina has become detached, you will need surgery. The operation may restore most of your vision but may come too late for a full recovery.
Look out for:
flashes or floaters getting worse
a black shadow in your vision
a sudden cloud of spots
a curtain or veil over your vision
any sudden loss of vision.
Unfortunately we can no longer assess you on the NHS under the Emergency Eye Care Scheme as this was decommissioned in the area. However we can assess you privately for a fee. Otherwise we recommend that you go to an Accident and Emergency Department without delay if you notice any of these symptoms.